Decoding the Importance of Methylated GBM: Understanding Treatment Response in Glioblastoma
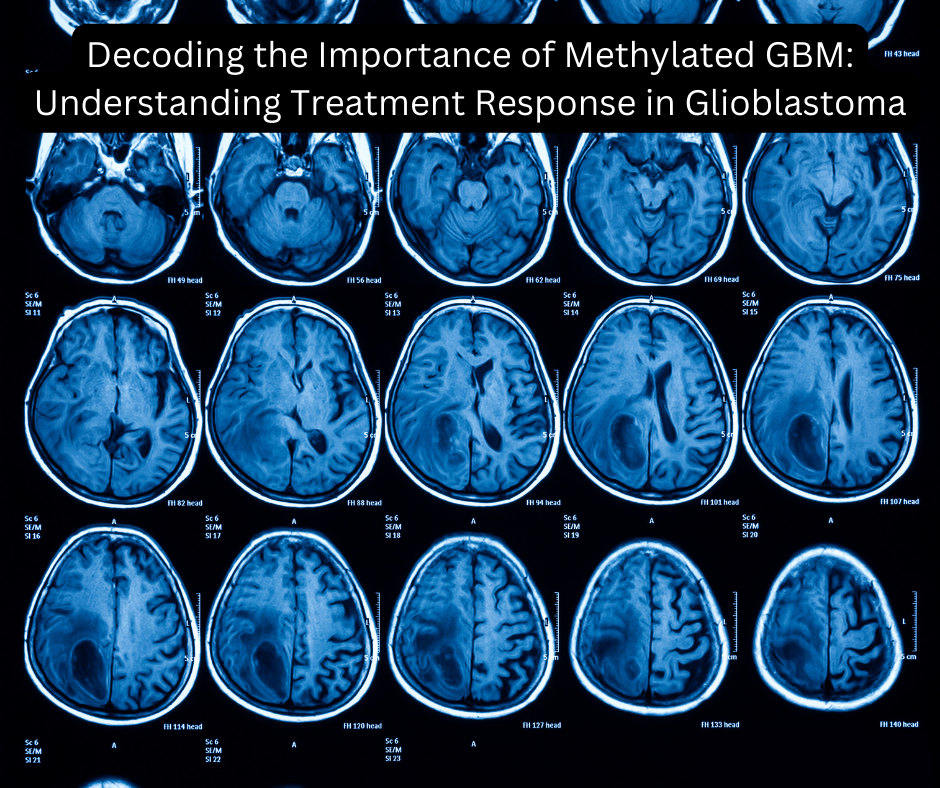
Decoding the Importance of Methylated GBM: Understanding Treatment Response in Glioblastoma
Living with glioblastoma (GBM) is not easy.
As a patient navigating through the complexities of this diagnosis, I have come across some intriguing research that sheds light on the intricacies of treatment options. Let me clarify—I am not a doctor. I am simply someone who is living with this disease and has spent countless hours digging into studies, patient forums, and clinical data in hopes of finding clarity—or at least a sense of control in this chaos.
So, what is all this talk about Methylated GBM being favorable over MGMT Unmethylated ?
It might sound like a bunch of intimidating medical jargon, but believe me, this distinction can carry real-world weight when it comes to prognosis and treatment planning.
You will often encounter these terms in discussions about the NeoTYPE™ Discovery Profile for Solid Tumors .
This comprehensive profile includes 326 genetic markers and utilizes advanced technologies such as Next-Generation Sequencing (NGS) , Fluorescence In Situ Hybridization (FISH) , and Immunohistochemistry (IHC) . These sophisticated tools are used to detect genomic alterations and molecular markers that can influence how certain tumors behave—and how they might respond to different treatments.
Now, let us unpack the science behind this.
The methylation status of the MGMT gene promoter is a key factor in determining how well a glioblastoma tumor will respond to standard therapies. MGMT stands for O6-methylguanine-DNA methyltransferase, a gene responsible for repairing damaged DNA in our cells. When this gene is active, it can actually work against certain chemotherapy treatments by repairing the very DNA damage those treatments aim to inflict on the cancer cells.
Here is where methylation comes into play.
When the MGMT promoter region is methylated , it means that small chemical groups—called methyl groups—have attached themselves to the promoter and effectively "silenced" the gene. In simple terms, the gene gets turned off. When the gene is unmethylated , it remains turned on and continues to repair DNA. This difference matters significantly when considering treatment response.
So, why should a GBM patient care about whether their MGMT gene is methylated or not?
Because multiple clinical studies have shown that patients with methylated GBM tumors tend to respond more favorably to treatment. Specifically, therapies involving temozolomide (TMZ) —a standard oral chemotherapy drug—combined with radiotherapy are shown to be more effective in this group. The presence of methylation means the MGMT gene is not actively fighting the effects of TMZ, allowing the drug to damage the tumor cells more effectively.
To put it plainly, MGMT methylation status is a powerful predictor of survival outcomes .
Those with methylated tumors often experience longer progression-free survival and overall survival compared to those with unmethylated tumors, who may have more resistant disease. This piece of information can be incredibly valuable when forming a treatment plan, and many oncologists now consider MGMT methylation testing a standard part of the GBM diagnostic process.
I remember vividly when I first came across this information.
It felt both empowering and overwhelming. On one hand, understanding my tumor’s genetic profile made the disease feel less like a faceless enemy and more like something I could at least try to understand. On the other hand, it was hard not to get consumed by statistics and survival rates. Every number carried weight, every percentage came with emotional baggage. It is a hard balance to strike—staying informed without drowning in dread.
But knowledge, as they say, is power.
Even though I cannot change my diagnosis, I can arm myself with information. I can ask better questions. I can advocate for the best care. Knowing whether my tumor is methylated helped guide the conversations I had with my neuro-oncologist. It helped me feel seen—not just as a patient with a brain tumor, but as an individual with a specific biological profile that deserved a tailored approach.
Of course, we must remember that science evolves .
What we know today may shift tomorrow. And while MGMT methylation status is an important factor, it is only one piece of a much larger puzzle. GBM is notoriously complex, and researchers are still uncovering new mutations, biomarkers, and pathways that could influence treatment in the future. Personalized medicine is the frontier we are all hoping for. A time when no two patients receive the same cookie-cutter treatment, but instead, precisely what their tumor requires.
But until we get there, knowing your MGMT status can help shape your path.
For those with unmethylated tumors, newer trials and alternative strategies may be considered—some involve immunotherapy, others novel drug combinations, or targeted therapies based on additional mutations. It may not be the news you want to hear, but it can spark action. It can lead you toward a clinical trial, a second opinion, or a new direction that you had not previously explored.
And let me say this again, loudly and clearly:
I am not a medical expert. I am just a human being trying to make sense of this disease, like so many others. Everything I write here is based on publicly available research, studies, and personal experience. Please consult your doctor or care team before making any treatment decisions. You deserve expert advice that considers your unique history and medical background.
Still, I hope that by sharing what I have learned, someone else might feel a little less in the dark.
This journey is brutal—but knowledge can be a small form of comfort. Understanding your tumor at the molecular level might not change the diagnosis, but it can illuminate the best way forward. And sometimes, that illumination is the difference between feeling helpless and feeling equipped.
In summary, the methylation status of the MGMT gene is a crucial determinant in how GBM patients respond to certain therapies.
When MGMT is methylated, standard treatments like temozolomide and radiation are often more successful. For unmethylated cases, doctors may consider alternative or experimental strategies. Either way, knowing your MGMT status allows you and your care team to make more informed choices.
If you or a loved one is facing a GBM diagnosis, I encourage you to ask about this test.
And if you have already had it done, take time to understand what the results might mean for your journey. GBM is a daunting diagnosis, but through research, resilience, and relentless curiosity, we can continue to push forward—one patient, one breakthrough, one day at a time.
You are not alone in this.

 NEW ARRIVALS
NEW ARRIVALS APPAREL
APPAREL GIFT AND HOME
GIFT AND HOME COLLECTION'S
COLLECTION'S HOPE HUB
HOPE HUB BLOG
BLOG